All about Batten Disease

What is Batten Disease?
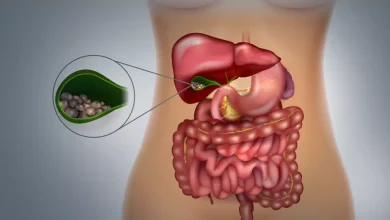
Batten disease falls under the umbrella disease. Umbrella disease is a term under which many neurological disorders come. Batten disease is not a single type of disease and it consists of various fatal genetic disorders. There are 13 types of batten disease which hampers our body’s capability to remove cellular waste like lipids and proteins from our bodies, and in response, they develop cells all over the body., This buildup leads to conditions such as seizures, blindness, mental disorders, movement of the, and at last it can cause death also.
What are The Types of Batten Disease?
Though there are 13 types of Batten Disease, though researchers have divided it into four major types on the basis of age, symptoms, and genes:
Infantile NCL (INCL) (CLN1): Infantile NCL (INCL) (CLN1) generally develops during the age of 6 months to 2 years. It may also result in microcephaly, along with jerks in the muscles. Most children who have INCL won’t live more than their mid-childhood period. There is also a puerile onset of CLN1, during the age of 5 to 6 when abnormalities start to develop. The progression of this disorder is usually not fast, rather it develops quite slowly. There is also a juvenile onset of CLN1, abnormalities develop around age 5/6 and disease progression is slower. Affected children may live into their teenage years or even into adulthood if they develop the symptoms during their puberty.
Late Infantile NCL (LINCL) (CLN2): LINCL ( abbreviation of Late Infantile NCL) generally begins between the ages of 2 and 4 and causes symptoms such as seizures and slowly losing the capability of walking and speaking. It’s a life-threatening type of batten disease where mostly the child having this disease dies between the ages of 8 to 12 years. No particular treatment can cure or back-pedal the symptoms of any type of Batten disease. Though an enzyme replacement therapy for CLN2 disease (TTP1 deficiency) is known as brineura. Brineura is a medicine that can slow down the loss of ability to walk among children of 3 years and older with late infantile neuronal ceroid lipofuscinosis type 2 (CLN2). Other than brineura there are no treatments available that can slow down or halt the development of diseases for other NCL conditions.
CLN3 disease: Juvenile onset (ages 4-7): In this type of batten disease, the children start to lose vision between 4 and 7 years. Problems of behavioral problems and learning begin, along with cognitive decline and children will start suffering from seizures during the age of 10 Seizures can be eased or decreased with anti-seizure medicines. After reaching adolescence they may get symptoms similar to parkinsonism. Even though medicines are available to treat the symptoms such as stiffness in the body along with problems with walking, sadly most children die between the age of 16 to 30.
Adult NCL (ANCL) (CLN4 or Kufs disease type B): This type of batten disease usually begins before early adulthood. People with these disorders will experience problems with movement and dementia but do not cause blindness. People who have Adult NCL (ANCL) have short life spans, but the time of death may differ from person to person.
What are The Symptoms of Batten Disease?
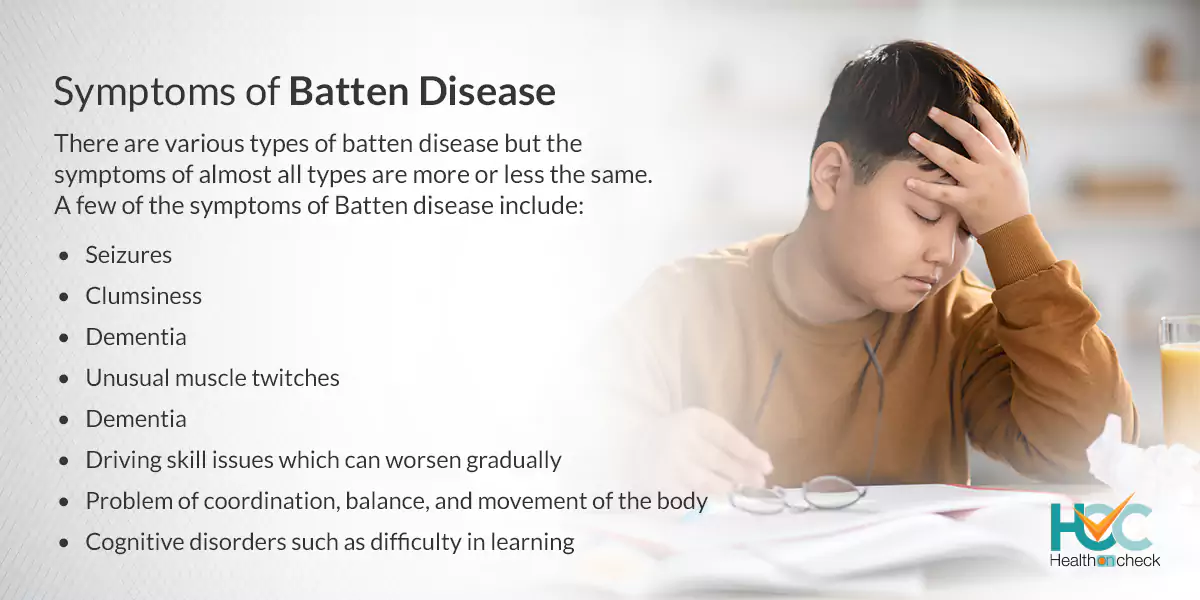
There are various types of batten disease but the symptoms of almost all types are more or less the same. A few of the symptoms of Batten disease include:
- Loss of vision
- Seizures.
- Cognitive disorders such as difficulty in learning.
- Speaking problems like stuttering, speaking very slowly, and repeating words or phrases again and again
- Clumsiness
- Problem of coordination, balance, and movement of the body
- Unusual muscle twitches
- Dementia
- Driving skill issues which can worsen gradually
What are the Causes of Batten Disease?
Batten disease is a genetic disease and you have a family history of this disease and inherited it through genes. This disease occurs only when both of your parents are carriers of a gene with a mutation. If an infant is born with it, then both parents have to carry genes that cause batten disease. The gene which is responsible for Batten disease damages the body’s capacity to break down and get rid of cellular waste. The amalgamation of fats, proteins, and sugar build up in cells all over the body mostly harms the brain cells which leads to stopping the functioning of the body.
What are the Risk Factors of Batten Disease?
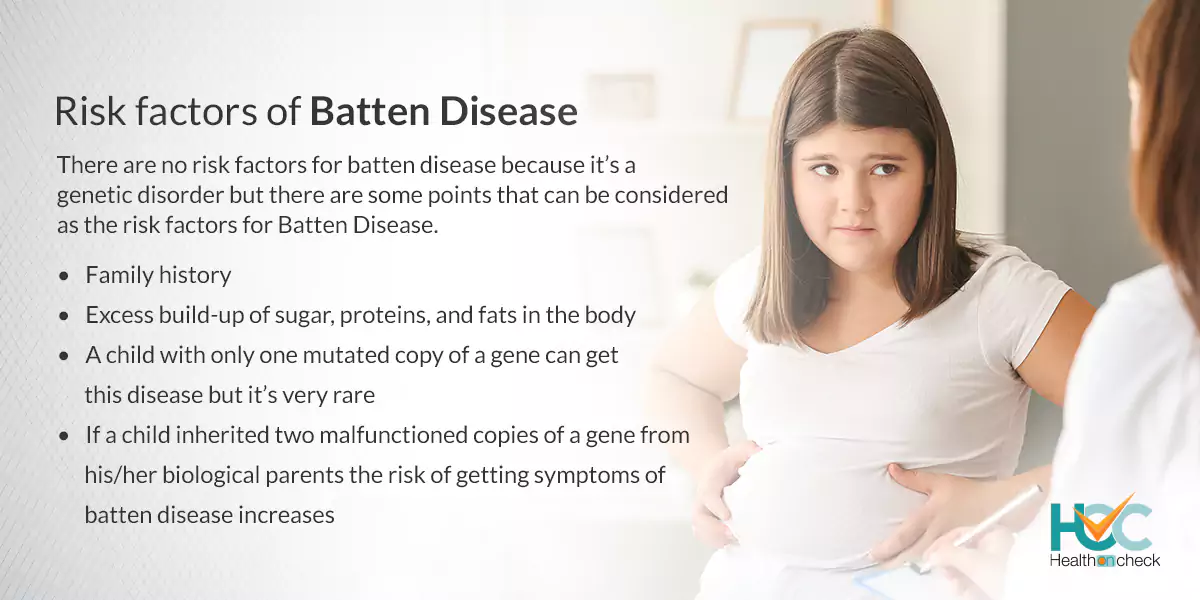
There are no risk factors for batten disease because it’s a genetic disorder but there are some points that can be considered as the risk factors for Batten Disease.
- Family history
- If a child inherited two malfunctioned copies of a gene from his/her biological parents the risk of getting symptoms of batten disease increases
- Excess build-up of sugar, proteins, and fats in the body
– A child with only one mutated copy of a gene can get this disease but it’s very rare
What are the Complications of Batten Disease?
The complications of batten disease vary because of there are almost 13 types of batten disease but some complications of Batten disease are:
- Blindness
- Slow development of body and brain
- Seizure attacks
- Pediatric neurodegenerative diseases
- Northern epilepsy syndrome
- Difficulty in walking
- Mental disorders such as having problems in thinking, forgetting things, etc
- Behavioural and learning problems
- Forgetting your own language
- Losing motor skills like driving and riding
- Death
How Batten Disease is Diagnosed?
The first step in diagnosing batten disease is talking with the patient and getting the patient’s family history. After this, some tests are recommended to make sure that it’s Batten Disease such as:
DNA Test: A sample of blood or saliva from the parents or the child will be taken and it will be sent to a lab. To study the DNA for mutations in genes. A DNA test can confirm whether one has batten disease or not.
Biopsy: A medical care provider will take a sample of tissue from the skin. It will then be examined in a microscope and checked for unusually big collections of lipofuscins. It will detect the amount of fats and proteins in the skin and other tissues.
Eye exam: A test known as electroretinography (ERG) will be taken to examine the condition of the optic nerve and retina along with checking how the retina is responding to light.
Blood or urine tests: Samples of your blood or skin may be taken to check for some particular types of abnormalities in blood and urine samples that can be a symptom of batten disease.
What are the Treatment Options Available for Batten Disease?
There is no treatment available to fully cure Batten disease, but some treatments can ease the symptoms of this disease along with helping the quality of life. But these treatments can’t cure or reverse the growth of the disease.
Treatment for the CLN2 subtype is available in a form of an enzyme replacement therapy known as cerliponase alfa (Brineura). It will slow or even avert the growth of the CLN2 subtype of batten disease but can’t treat other types.
Treatment options to ease the symptoms include:
- Anti-seizure medicines
- Anti-depression and anxiety medicines to treat mental disorders
- Medicines for parkinsonism
- Treating spasticity with some certain medicines
– Physical therapy and occupational therapy to slow down body-related conditions
Living With Batten Disease
People with batten disease do not live more and very rarely one can live up to forty years of age. Living with Batten disease is difficult for both patients and their parents and caretakers. With proper treatment, a healthy diet, and lifestyle changes, along with joining support groups, may help in coping with the mental and physical issues the patient is going through and maintaining a good quality of life.
Whom to Consult?
If you or anyone in your family including your newborn baby is showing signs and symptoms of batten disease then immediately consult a doctor and get yourself diagnosed if it’s batten disease or not and then start treatment accordingly. In addition, if you or your partner are batten disease patients or have a family history of Batten disease then give lots of time contemplating and discussing with your partner before deciding to be parents. Meet doctors who are specialised in this particular and take advice from and plan your pregnancy accordingly.