All about Tularemia

What is Tularemia?
Tularemia, also known as deerfly fever and rabbit fever, is a disease that is caused by the bacterium Francisella tularensis (F. tularensis) which makes your lymph nodes swell painfully along with other symptoms in your eyes, lungs, eyes, and intestines, based on where the bacteria has infected you. It is a zoonotic disease, meaning it can spread from animals to humans. People usually get tularemia after being exposed to deer flies and ticks that have F. tularensis infections, that is why it’s also called deerfly fever. You might also get this disease after getting in contact with infected animals, usually such as rabbits, hares, and rodents, or food and water sources that are contaminated with the bacteria.
What are the Types of Tularemia?
Tularemia has various types, based on how you got infected with F. tularensis and your systems. The types of tularemia include:
Ulceroglandular tularemia: It is the most common type of tularemia which you generally get after getting bitten by a tick or an infected animal. Your skin and lymph nodes are affected by it.
Glandular tularemia: Glandular tularemia is the same as ulceroglandular tularemia, and the difference is that it affects only your lymph nodes and not the skin. You can get glandular tularemia after being bitten by a tick or directly from an infected animal.
Oculoglandular tularemia: Contaminated water or body fluids in your eye may cause oculoglandular tularemia which leads to symptoms in and around your infected eye. Oculoglandular tularemia normally doesn’t affect both eyes.
Oropharyngeal tularemia: You can get oropharyngeal tularemia by consuming contaminated food, or water, or touching your hands to your mouth without washing them. The main symptoms include sore throat and sometimes digestive (gastrointestinal) symptoms.
Pneumonic tularemia: It is the most severe type of tularemia and its symptoms are similar to pneumonia. You might get pneumonic tularemia in two ways:
Breathing in F. tularensis: tularensis can spread to your lungs from other parts of your body.
Typhoidal tularemia: Typhoidal tularemia leads to a high fever and impacts various areas of your body. You may get typhoidal tularemia the same way as other types of tularemia.
What are the Symptoms of Tularemia?
Symptoms of tularemia are based on the type. Most types result in a fever, many forms of rash along with additional symptoms specific to where the infection is in your body.

Symptoms of ulceroglandular and glandular tularemia
- Fever.
- Very huge, painful, and swollen lymph nodes.
- Open wound on your skin.
Symptoms of oculoglandular tularemia
- Eye pain.
- Watery eyes.
- Sensitivity to light.
- Painful, swollen lymph nodes near your neck or ears.
- Open sore on your eye.
Symptoms of oropharyngeal tularemia
- Fever.
- Severe sore throat.
- Red, swollen throat with white patches.
Some people might also suffer from:
- Vomiting.
- Diarrhoea (sometimes bloody).
- Abdominal pain.
Symptoms of pneumonic tularemia
- Fever.
- Cough.
- Shortness of breath.
- Tightness or chest pain.
- Muscle aches.
- Red bumps or rash (erythema nodosum).
- Blood in cough.
Symptoms of typhoidal tularemia
- High fever.
- Chills.
- Headache.
- Loss of appetite.
- Muscle pain.
- Sore throat.
- Abdominal pain.
- Diarrhoea.
- Nausea
- Vomiting.
- Confusion.
What are the Causes of Tularemia?
Tularemia is caused by the bacterium F. tularensis which resides in animals generally hares, rabbits, deer, rodents, and cats along with ticks and other biting insects that also carry it.
There are two forms of F. tularensis, type A and type B. Type A causes more severe illness, and type B causes mild symptoms.
Tularemia is transmitted in various ways. You may get tularemia from:
- Bites from ticks, mosquitos, deer flies, and other biting insects.
- Bites from infected animals.
- Getting in contact with infected animals by touching them. In case you touch the infected tissue or body fluids of an animal, it can enter your body through breaks in your skin. You may also get it in your eyes, nose, or mouth if you touch your face after contact with F. tularensis.
- Consuming contaminated food.
- Breathing in an aerosol (mist) with F. tularensis in it. It might occur if a lawn mower or piece of farming equipment runs over an infected animal.
What are the Risk Factors of Tularemia?
Tularemia is rare and people usually get it from tick bites or contact with a contaminated animal.
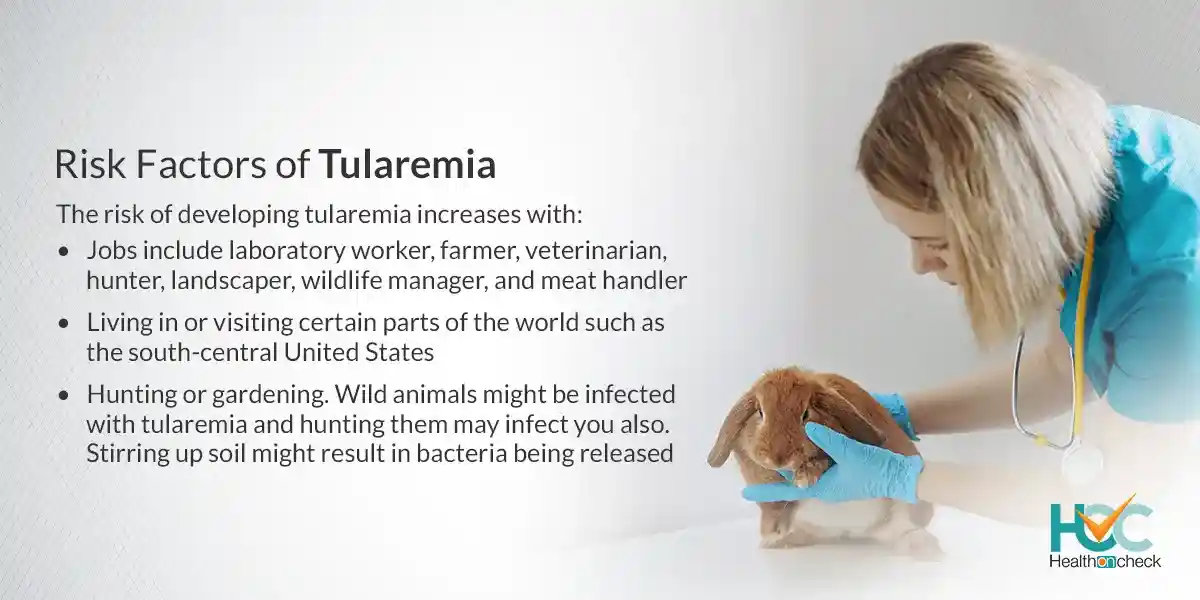
The risk of developing tularemia increases with:
- Jobs include laboratory worker, farmer, veterinarian, hunter, landscaper, wildlife manager, and meat handler.
- Living in or visiting certain parts of the world such as the south-central United States.
- Hunting or gardening. Wild animals might be infected with tularemia and hunting them may infect you also. Stirring up soil might result in bacteria being released.
What are the Complications of Tularemia?
Complications of tularemia include:
- Acute respiratory distress syndrome (ARDS).
- Brain inflammation.
- Heart inflammation.
- Bone, bone marrow, or joint inflammation.
- Liver inflammation.
- Kidney (renal) failure.
- Internal bleeding (haemorrhage).
How Tularemia is Diagnosed?
To diagnose tularemia, your doctor will first examine you, get information about your symptoms along with testing your blood or other body fluids. Based on your symptoms, they may examine your lymph nodes, your throat, your eyes, and any ulcers, bumps, or rashes you may have on your skin.
Tests to diagnose tularemia include:
Blood tests: Your blood sample will be taken and sent to a lab. The lab will detect signs of tularemia and may examine if F. tularensis grows from it. At first, your blood test might seem normal because F. tularensis can be slow-growing. You might have to repeat blood tests some weeks later.
Biopsy: If you have large lymph nodes or ulcers, a sample of your tissue will be taken and sent for biopsy. A lab will examine the sample for F. tularensis or check if it grows from the sample.
Nasal or throat swab: A long stick with a soft tip (swab) might be used by your doctor to get a sample of mucus from your nose or throat and it will be sent to a lab to check for F. tularensis or examine if it grows from the sample.
Pleural fluid test (thoracentesis): If you have fluid near your lungs, your doctor might take its sample during a thoracentesis and send it to a lab for testing to see if it grows from the sample.
What are the Treatment Options Available for Tularemia?
Treatment of tularemia includes giving broad-spectrum antibiotics, either through a needle (injection) or orally (pill). You also might require other treatments if you have severe complications.
It’s quite vital to treat tularemia immediately after getting diagnosed. Your doctor might give you antibiotics before your test results are back to keep you from getting severely ill.
Antibiotics given to treat tularemia include:
- Streptomycin.
- Gentamicin.
- Doxycycline.
- Azithromycin.
- Ciprofloxacin or levofloxacin.
Living with Tularemia
People with tularemia usually make a full recovery and you can expect to be on antibiotics for one to three weeks.
Based on your symptoms, your doctor might monitor you closely for the first few days of treatment. If your symptoms start a while before beginning antibiotics, you might have serious complications.
Some people’s symptoms return after they start to feel better and if it occurs to you, you may have to take another course of antibiotics.
Whom to Consult?
Tularemia is a rare but serious condition and if you think you were exposed to or have symptoms of tularemia, you should seek medical help right away. With fast treatment, a full recovery is possible.